Executive Summary
The Nordic Charter for Women's Health 2040 is a strategic framework designed to transform women's health from a niche concern into a cornerstone of Nordic social and economic resilience. Resulting from the collective insight of over 130 contributors across Denmark, Norway, Sweden, Finland, and Iceland, gathering at Danish Parliament Sept. 8th 2025, this document moves beyond aspiration to outline a concrete infrastructure for systemic change. This Charter embodies the collective insight, ambition, and commitment to shaping a Nordic future where women's health is systemic, equitable, and inclusive.
The Strategic Imperative
By 2040, the Nordic region will face a profound demographic shift, with millions of women navigating menopause and aging simultaneously. This presents a clear choice: accept rising healthcare costs and lost productivity, or proactively invest in a Health Resilience Economy. Closing the women's health gap offers a potential USD 30–50 billion annual opportunity in productivity gains and innovation in the Nordics.
The Vision
We envision a future in 2040 where women's health is anticipatory, data-driven, and integrated into everyday wellbeing, a reality where health is a birthright, not a benefit. This Charter serves as both the map and the mandate to build that future, positioning the Nordics as the global standard-bearer for equality in health.
A Framework for Coordinated Action
This Charter replaces fragmented efforts with a unified coordination matrix. It identifies three operational domains (Research, Care, Innovation) supported by four shared Infrastructure Pillars:
- People (Capacity & Training): Building a workforce trained in female physiology.
- Money (Funding & Investment): Shifting from episodic spending to life-cycle budgeting.
- Policy (Governance & Regulation): Mandating sex-disaggregated data and inclusive standards.
- Data (Infrastructure & Standards): Creating a shared Nordic data layer.
Underpinned by a foundation of Awareness, this framework enables governments, institutions, organisations across the private and public sector, and investors to align their actions without requiring centralised control.
Immediate Opportunities
The Women's Health 2040 Framework identifies coordination opportunities across all domains and pillars. Institutions can begin engagement immediately, research councils through funding alignment, health systems through measurement pilots, innovation agencies through regulatory coordination, education ministries through curriculum review. The detailed mapping of specific initiatives against existing Nordic and European efforts continues as the next phase of Charter development.
Editor’s Note
This Charter is published as an open commons, deliberately free from proprietary ownership so that every researcher, clinician, policymaker, innovator, and citizen across the Nordic region can build on it, and use it to enhance their work in women's health. Open commons governance is uncommon in health policy, yet it is precisely what is required to enable radical, cross-sector innovation in women's health. This openness is part of one of the 360 degree design principles in the process, ensuring a holistic view of women's health, across sectors and national borders. This vision is designed to raise the bar for women's health, pushing all sectors to think bigger, act bolder, and collectively redefine what is possible for women's health by 2040.
Part 1
Why This Matters
Introduction
Across the Nordics, clear signs of change show a real opening for progress in women's health. Activity is already rising, across research, clinics, innovation, and policy, indicating a need for coordination to trigger potential synergy. Women's health now represents a defining choice for the region: the current reality of lower healthy life expectancy, years-long diagnostic delays, and research that overlooks female physiology is neither inevitable nor acceptable.
Women in the Nordic region, as elsewhere, live longer but spend significantly more years in poor health than men; globally, women spend about 25% more of their lives in poor health than men. Yet only around 5% of global health R&D funding is dedicated to women's health, and just 1% to non-oncology women-specific conditions. In a nationwide study of 6.9 million people, women were diagnosed about four years later than men across 770 non-sex-specific diseases. Together, these gaps show how limited our understanding of women's biology and health still is.
The Nordics have every advantage needed to lead, world-class institutions, universal healthcare, strong governance, and populations demanding evidence-based equality. This Charter captures those signals and offer a permissive coordination tool and menu of options. It outlines the key systemic shifts and a shared frame through which institutions may choose to align, adapt, and build on what exists, at their pace, in their context. The aim is practical: enable multiple pathways toward women's health that are equitable by design, integrated across life stages, and part of everyday wellbeing, without prescribing a single route or imposing obligations. The document also integrates a narrative case, ‘Nora’s Life in 2040’, illustrating how future systems are experienced in daily life across an entire life course, grounding the vision in lived reality.
Each stakeholder working with women's health can advance the vision in ways that fit local context. The Charter outlines three systemic transformations and provides a coordination framework (3 missions × 5 infrastructure pillars) that maps existing initiatives and identifies opportunities for alignment and investment. It enables, rather than prescribes, national and institutional strategies, offering a common reference for governments, research bodies, and innovation ecosystems to coordinate toward a shared Nordic horizon: health that is equitable by design, integrated across life stages, and woven into everyday wellbeing. Used this way, the framework helps convert dispersed efforts into systemic change and makes women's health a durable strength of the Nordic model.
1.1Purpose of the Charter
The Nordic Charter for Women's Health 2040 serves as a shared framework for collaboration and transformation across research, care, innovation, governance, and public awareness. Its purpose is to connect existing initiatives, inspire new ones, and guide collective action toward a future where women's health is a birthright, not a benefit.
The Charter functions as both a shared map and a menu of initiatives. It can be used flexibly to inform national strategy development, enable targeted institutional partnerships, or guide individual initiative selection. No single coordination body is required, though the framework supports coordinated action if institutions choose to pursue it. This Charter is intended to complement existing national health strategies, clinical guidelines and professional standards, serving as a shared direction rather than a parallel framework.
Rather than prescribing national policies, the Charter aligns diverse efforts and cross-cutting transformations, ensuring that collective, simultaneous action across sectors accelerates both the pace and quality of systemic change. It invites governments, institutions, and communities to translate these principles into context-specific strategies, ensuring that by 2040, women's health becomes a defining measure of equality, wellbeing, and sustainable progress across the Nordic region.
1.2Definition of Women’s Health
When we talk about women's health in the context of Vision 2040, it is grounded in biological sex, recognising the distinct health needs of female bodies across the full life course, from childhood to puberty and fertility to menopause and ageing. Yet women's health is also shaped by societal structures: by institutions, workplace conditions, caregiving responsibilities, health system design, data gaps, culture and policy blind spots.
At the same time, we recognise that womanhood is experienced in diverse ways. Our framing includes every woman, in all her diversity, across identities, bodies, cultures, and life circumstances. In this sense, women's health is understood as the intersection of biology and society, determined as much by prevention and equity as by diagnostics, treatment, and systemic design.
With this framing, we treat women's health not as a niche issue, as the dominant narratives have been portraying women so far, but as foundational infrastructure for equality, wellbeing, and economic resilience across the Nordic region.
Note on Scope & Inclusivity
This definition focuses on women's health as an area that has long been overlooked in research, innovation, and healthcare systems. It does not seek to exclude or erase other gender identities or population groups, but to centre those whose specific biological and structural health needs have historically been underrepresented and undervalued.
1.3Why Now?
Women's health is not an individual matter, it's a societal one.
The case for transforming women's health in the Nordics has never been stronger. Demographic change alone makes it urgent: By 2040, ⅓ of Nordic women are expected to live beyond 100 years on average, spending nearly half their lives in menopause. Without a shift from late treatment to prevention, health systems will face unsustainable costs, and women will continue to experience avoidable suffering.
The Cost of Inaction
Unsustainable healthcare burden driven by aging demographics and more years lived in poor health.
The Economic Prize
USD 30–50 billion annually in Nordic productivity, reduced healthcare costs, and innovation growth.
The Wealth Transfer
A share of the global USD 30–68 trillion intergenerational wealth shift, with women projected to control USD 30 trillion in the U.S. alone by 2030.
The economic argument is equally compelling. The financial value of women's unpaid domestic and care work amounts to around USD 10.8 trillion per year. That's three times more than the global tech industry. Closing the women's health gap could unlock USD 30–50 billion annually in the Nordics through productivity gains, reduced healthcare costs, and new markets for innovation.
At the same time, scientific breakthroughs are arriving at a rapid pace. AI, digital twins, precision medicine, and organ-on-chip technologies have the potential to revolutionise care. Yet if they are developed on today's biased datasets, they risk repeating the exclusions of the past. When we feed AI with historical and human bias, we risk accelerating the very inequalities that have held women's health back, turning yesterday's blind spots into tomorrow's systems. Data development should include validated outcome measures, shared terminology and quality indicators to support comparison across countries and research settings.
The cultural tide is also turning: younger generations are breaking the silence around menstruation, fertility, and menopause, demanding openness, literacy, and agency. Governments now have a unique policy window to respond. The Nordics, with their legacy of leadership in equality and sustainability, can set the direction for EU directives and WHO standards, but only if they act now and consistently.
Europe is at a tipping point in women's health. On one hand, the FemTech ecosystem is growing fast, projected to reach USD35 billion by 2032. Startups founded and cofounded by women actually performed better over time, generating 10% more in cumulative revenue over a five-year period: USD730,000 compared with USD662,000. On the other hand, female-founded startups still raise only half the capital of their male counterparts, leaving the field structurally underfunded.
The Great Wealth Transfer refers to how an estimated USD30–68 trillion will shift from Baby Boomers to younger generations globally by 2030. In the U.S. alone, women are projected to control USD30 trillion in assets by 2030, due to inheritance, divorce, and longer lifespans. In Europe, women will inherit an even greater share, as they increasingly outlive male partners and become primary heirs. If even 1% of this USD30 trillion were directed toward women's health innovation, it would dwarf today's total FemTech investment. That level of capital would allow us to close the research gaps in menopause, maternal health, the female endocrine system, women's metabolism, and chronic diseases that disproportionately affect women, as well as advance research on sex-specific diseases.
In other words, this is the decade to mainstream women's health as a defining investment frontier. The Charter for Nordic Women's Health 2040 is a rallying point to ensure that this unprecedented transfer of capital and decision-making power is aligned with the most urgent and transformative opportunity of our time.
1.4How to Read This Document
This Charter is organised into four parts:
Part 1: Why This Matters
Provides context on the opportunity, urgency, and definition of women's health that grounds the framework.
Part 2: The Shared Vision
Presents the 2040 vision through aspirational framing and a lived-experience scenario (Nora's story), stress-tests it against strategic uncertainties, and defines three systemic transformations.
Part 3: The Women's Health 2040 Framework
An integrated 3×4+1 matrix structure that brings together the insights from the five expert groups. Already at this stage, you can orient yourself toward this framework as the structural focal point of the document.
Part 4: Pathways Forward
Describes multiple ways institutions can engage, from coordinated Nordic strategy development to bilateral collaboration, individual initiative selection, or funding alignment, and outlines next steps for detailed mapping.
How to Use This Charter
Policymakers and ministries
Can use the framework to identify where national strategies align with Nordic priorities, which coordination opportunities exist, and where independent action makes sense (see Part 3.3 for matrix structure, Part 4.1 for engagement pathways).
Research and innovation institutions
Can identify specific entry points within the matrix that match institutional strengths, whether establishing sex-stratification mandates, building data infrastructure, or launching training programmes (see Part 3.2 for the convergence table).
Funders and investors
Can use the matrix to identify strategic priorities, understand where coordinated funding unlocks systemic change versus where targeted investments enable specific initiatives, and align resources with enabling infrastructure (see Part 4.1 for funding alignment pathway).
Coordination bodies
Considering Nordic cooperation can assess which matrix cells benefit most from joint action, where bilateral collaboration might move faster, and how to balance coordination with institutional autonomy (see Part 3.3 for how the Women's Health 2040 Framework works, Part 4 for implementation options). At the same time, women's health researchers and companies can use the framework as an additional reference point when advocating for greater prioritisation, funding, and visibility for women's health across the Nordics.
The framework is intentionally flexible. Organisations can draw on the elements most relevant to their mandate without adopting the full structure, and even partial use can contribute to systemic transformation when multiple actors align within the same coordination logic.

Part 2
The Shared Vision
2.0A Vision for Women’s Health 2040
This chapter presents the Vision for Women's Health 2040, the shared outcome of strategic foresight work with the Copenhagen Institute for Futures Studies and Nordic Women's Health Hub, real-time insights gathered from participants through a live survey at the Danish Parliament, and the collective reflections of experts across five expert groups. Together, these inputs form a rich foundation for futures thinking, lived experience, and professional expertise, reimagining what good health standards for women will look like across the Nordic region by 2040.
2.1A Vision of the Future
“By 2040, every woman in the Nordics lives in a society where health is a birthright, not a benefit, anticipated, equitable, and seamlessly woven into everyday life.
| Not a benefit | Anticipated | Equitable | Seamlessly woven |
|---|---|---|---|
| Health is no longer something she must fight for, but something she simply lives. | A woman moves through life supported by systems that anticipate her needs. Our systems are anticipatory, data-driven, and rooted in lived experience. | Supported by equitable research, personalised women-centred care, inclusive innovation, universal health literacy, and preventive policy. | Respects her biology, and value her wellbeing as self-evident, enhancing quality of life for individuals, households, communities, and societies. |
2.2Women’s Health 2040: A Future Scenario
The year is 2040, and fifteen-year-old Nora walks into her school's health literacy class, calm and curious. Around her, laughter echoes, not nervous giggles or whispers, but open, confident conversations about topics that once hid behind closed doors: menstruation, fertility, hormonal and mental health. Her teacher begins with a simple statement:
“You will likely live to be one hundred. To the ladies in the room, you are likely to spend nearly half your life in post-menopause. The key is to live it well.
Nora listens, taking notes on her digital tablet that syncs seamlessly with her personal health record. Her device already knows her basic hormonal patterns, inherited predispositions, and even her sleep cycles. It doesn't diagnose, it guides. It nudges her when to rest, when to hydrate, and when to move. It's not surveillance, it's empowerment. For Nora's generation, poor health isn't something that happens to them; it's something they learn to prevent and manage.
Nora's classmate, Elias, never had to unlearn the idea that women's health was 'none of his business'. In his world, understanding menstruation, fertility, menopause and hormonal health is part of being an informed citizen, a competent future partner, colleague and leader. For Nora's teacher, Johan, this cultural shift did not come easy. He grew up with a quality paradigm that said: if men and women are equal, you must treat them exactly the same. Asking for sex-specific data or cycle-aware policies once sounded, to him, like going backwards.
A Society That Learned to Listen
At home that evening, Nora's grandmother, Sara, joins the family for dinner. She's seventy-two now, radiant and full of stories. When I was your age, she says,
“We didn't talk about periods at all. Doctors told me cramps were in my head, that I was overreacting as menstrual cramps can't be that bad, and that every woman has them.
Sara remembers when the first wave of reform began back in the 2020s. Laws changed after women's advocates exposed decades of bias in research and care. Governments passed the Nordic Charter for Women's Health 2040, declaring that sex-disaggregated data and inclusive testing were not optional; they were mandatory.
Medical schools rewrote curricula, ensuring every doctor understood female biology as thoroughly as male physiology. Health ceased to be reactive; it became preventive, anticipatory, and equitable. Doctors' incentive structures used to be paid per patient seen, but today it is a value-based care model that rewards them for keeping the population healthy.
When Sara's heart was first monitored through a hormonal health care programme in her sixties, her data automatically fed into the national health system, anonymised, secure, but useful. The Nordic Health Data Framework linked every Nordic country through interoperable, ethical data-sharing standards. Trust, built through transparency and co-ownership, became the region's competitive advantage.
Now, when Nora visits her school nurse for irregular cycles, she isn't dismissed or medicated by default. Instead, the nurse uses the digital twin in Nora's health record to simulate how her body might respond to changes in nutrition, sleep, or stress. Together, they create a personalised prevention plan. It's standard practice, and a daily reminder of how political will, legal reform, and ethical innovation built a system that listens to real world experiences.
Innovation With Integrity
Across the Nordics, female-led innovation ecosystems drive what economists now call the “Health Resilience Economy.” What began as a small femtech movement has grown into a multi-billion-euro sector, one that thrives on inclusive design, ethical AI, and preventive health technologies.
Nora's mother, Alma, is part of that ecosystem. She works for a company developing AI-driven hormonal health assistants, technology that integrates physical, emotional, and cognitive data into adaptive care models. Her team collaborates with public hospitals and universities, no longer competing, but co-creating under a shared framework that rewards long-term well-being over short-term profits.
Investors now measure Return on Inclusion (ROI): the combined value of efficacy gains, healthcare lifetime savings, and social cohesion. And social cohesion includes future generations. Any negative impact on climate or biodiversity ultimately harms the population of tomorrow, and the evidence shows that women are likely to be hit proportionally harder than men. That is why this is included when ROI is estimated. Doing good for today's population cannot come at the expense of the next. Economies no longer separate ethics from economics; they've learned that women's health is both a moral imperative and a growth strategy. Alma often says, “I remember the time when we stopped designing around symptoms and started designing around lives.”
Breaking Silence, Building Knowledge
Socially, everything has changed, though not without effort. The shift from taboo to transparency took two decades of media reform, education policy, and community investment. Nordic schools now treat health literacy as a core curriculum, taught alongside languages and science. By age ten, every child, boy or girl, can name basic hormonal stages and understand how lifestyle affects their state of health.
Nora's classroom discussions are paralleled in her father's workplace seminars. Companies have cycle-aware policies, menopause support programmes, and parental leave structures that accommodate all genders. Men attend workshops on reproductive and hormonal health, not only as allies, but also as active participants in a shared social contract.
Planetary Health, Personal Connection
The summer of 2035 was a turning point. Nordic governments had already acted on research showing that rising infertility rates and hormonal disorders were linked to microplastics and endocrine-disrupting chemicals, and by 2035 the results of that action were finally visible; hormone-related conditions stopped rising, and early biomarkers of endocrine disruption dropped across population studies. Women-led organisations had spearheaded alternative products to plastics, incentivised circular manufacturing, and embedded women's health metrics into environmental assessments.
Now, in 2040, sustainability and women's health are inseparable. Cities design green zones to reduce heat stress on pregnant women. Regulatory impact assessments showed that integrating a gender-sensitive health lens into environmental and food policy could prevent tens of thousands of hormone-related disorders and save billions in healthcare costs each year.
The Law as Guardian, Not Gatekeeper
The political and legal landscape of Nora's world is almost unrecognisable to her grandmother. The old patchwork of national systems has evolved into a Nordic Health Governance Network, harmonised across borders. Policies no longer lag behind innovation; they evolve with it.
Every new medical device or AI platform must meet inclusive testing and explainability standards. Citizens retain ownership of their data, consenting dynamically to how it's used. Instead of cumbersome regulation, agile charters and public dialogues ensure accountability.
A Culture of Prevention
Years later, Nora will look back and realise that her generation was the first to grow up seeing health not as crisis management, but as a lifelong practice of prevention.
Her grandmother's era fought for recognition. Her mother's generation built the infrastructure. Nora's generation lives the results, guided by data, supported by policy, and sustained by culture.
She will likely live to one hundred, half of those years post-menopause. Yet she feels no fear, only readiness, cause she knows how to handle it. And somewhere deep inside, Nora knows that her grandmother's words were true:
““We built this future so you wouldn’t have to fight for basic care in natural transitions in life.”
2.3Stress-Testing the Vision
Nora's world in 2040 illustrates what the Nordic region can achieve when science, policy, and culture align toward a shared purpose. Yet even a preferred future must navigate uncertainty. As a normative scenario, the Vision does not seek to predict or test probabilities; it defines what should be achieved. Nevertheless, this envisioned future must be considered in relation to the external forces and strategic uncertainties that could shape or constrain the pathway toward it.
Political shifts, economic pressures, technological disruptions, wars, environmental or climate disasters, and social change all have the potential to accelerate or undermine progress. Understanding these dynamics is crucial for designing policies, partnerships, and governance frameworks that can adapt to evolving conditions and keep the 2040 Vision on track.
Three Key Strategic Uncertainties
1) Governance Fragmentation
Nordic collaboration is the foundation of this vision. If political consensus weakens, or if public trust in data systems declines, collective progress could stall. Fragmented approaches would risk unequal access and widening gaps between nations, especially affecting rural and marginalised populations.
2) The Risk of Inequality by Design
Technological progress will keep accelerating, but if inclusive and representative datasets don't evolve alongside it, the data gaps will only grow. Inclusion doesn't happen by itself. If women's health tools, AI systems, or digital platforms remain accessible only to certain groups, even when built on representative datasets, the very equity that defines the Nordic model risks eroding. Making sure every innovation is grounded in representative data and designed for diversity and affordability is therefore a core resilience task.
3) Cultural And Financial Inertia
Even with strong policy and innovation, transformation can slow if social attitudes and funding priorities remain static. Persistent taboos, limited investments, or competing agendas could keep women's health under-prioritised. Without cultural openness and sustained resources, ambition risks fading into symbolism.
Leverage Points for Resilience
Each uncertainty points to where resilience must be built, through policy, trust, inclusion, culture, and shared value creation. The following levers define how the Nordic region can safeguard progress and keep the Vision alive under changing conditions:
A Strong Policy Backbone
Sustained political alignment and a shared Nordic framework, such as this Charter, ensure coherence and collective accountability.
Trust in Data And Governance systems
Public trust must be continuously earned through transparency, citizen ownership, and ethical use of health data.
Inclusive Design And Innovation
Health technologies and solutions should be designed for diversity, ensuring that e.g., ethnic minorities, sexual minorities, people with disabilities, elderly women, rural populations, and low-income groups benefit equally.
Cultural Transformation
Scientific progress must be matched by social openness, supported through education, awareness, and inclusive dialogue that dismantles stigma and silence.
A Visible Economic Narrative
Positioning women's health as a USD 30–50 billion Nordic opportunity maintains political and investment commitment, reframing equity as both an ethical and economic imperative.
These insights confirm that the Vision for Nordic Women's Health 2040 is both plausible and achievable, but only through deliberate, coordinated action. The uncertainties are not barriers but signals: they highlight where resilience must be built and vigilance maintained. A strong policy backbone, ethical data systems, inclusive innovation, cultural openness, and a shared economic rationale together form the foundation for sustained progress toward the 2040 horizon.

Part 3
From Experts’ Insights to One Unified Framework
3.1The Breakthrough: How Five Became Three Plus Four Plus One
The future Nora experiences in 2040 is not a coincidence; it is the result of actions taken today. Her preventative care was made possible by digital twin technology trained on datasets mandated by 2026 legislation. Translating Vision 2040 into concrete action requires structures capable of carrying that transformation. The five expert groups independently identified the same systemic building blocks, and these form the foundation of the Women's Health 2040 Framework. This section outlines the machinery required to build that reality and shows how the coordination framework emerged from the convergence of their insights.
In September 2025, 50 experts across five Nordic countries gathered at the Danish Parliament to envision women's health in 2040. They worked in five expert groups: Equitable Research, Women-Centred Care, Inclusive Innovation, Innovative Governance, and Health Literacy & Awareness. Each group developed transformations, activities, and success metrics for their area. We expected five separate action plans. What emerged was something more powerful: a coordinated framework.
The Insight: When we mapped the activities across all five groups, a striking pattern appeared. Governance and Literacy weren't separate competing priorities — they were the enabling infrastructure that Research, Care, and Innovation all require. Every group independently identified the same needs: training professionals, securing funding, establishing regulations, and building data systems. The difference was only the lens through which they saw those needs.
This revealed the framework's true structure:
| Element | What It Is | Components |
|---|---|---|
| 3 Domains | Operational areas that deliver results | Research, Care, Innovation |
| 4 Pillars | Shared infrastructure enabling all domains | People, Money, Policy, Data |
| 1 Foundation | Cultural enabler that makes everything possible | Awareness |
Table 1: Framework Structure
Section 3.2 presents what each expert group developed — their vision, transformations, and roadmaps. Section 3.3 then reveals the pattern that emerged when we mapped these outputs together, leading to the 3×4+1 framework that organises the rest of this Charter.
3.2What Five Expert Groups Discovered
Using participatory strategic foresight methodology, each group identified what must be true by 2026, 2030, and 2035 for the Vision to become reality by 2040. They developed transformational shifts and proposed activities to achieve them. Their findings follow.
Equitable Research
Mission Statement
By 2040, Nordic equitable research will secure sustainable efforts to guarantee women's health R&D that transforms society through coordinated research leadership, validated methodologies producing high-quality data reflecting female health, and EU-scale funding mechanisms that provide critical mass for breakthrough discoveries moving from symptom management to root cause treatments.
The Research group identified three critical transformations. Research leadership must shift from funding directed to established norms toward fundamental female physiology with equitable investment. Methodology must evolve: We need to move from relying on incomplete and insufficient female health data in AI and machine learning to building systems on high-quality female health data that reflects real-world experience. Funding requires transformation from fragmented European funding misaligned with women's disease burden to a European Women's Health Joint Undertaking ensuring sustainable, long-term funding. Their roadmap prioritizes communicating gaps and highlighting societal relevance (2025-2027), mandating female inclusion in research with proportional funding allocation (2030-2035), culminating in an EU platform for sex-stratified randomized controlled trials and whole-person, life-cycle research by 2040.
Women-Centered Care
Mission Statement
By 2040, women in the Nordics will benefit from superior quality of life with well-funded and well-designed healthcare supporting every life stage. Efficient, preventative and personalised care driven by cross collaboration, embracing technology advancements, and deep expertise in women's health will set a new global standard for women-centric healthcare.
The Care group emphasised three transformative elements. A focus on quality-of-life metrics requires developing and implementing standardised tools for measuring quality of life, such as the EQ-5D-5L. This shift ensures that care is prioritised in ways that make longer lives better lives. Protecting equity and leading through education requires educating healthcare gatekeepers and the public while influencing politics to embed women's health as a policy priority. Articulating solutions means defining problems caused by gender bias in detail, estimating the benefits of addressing them, and providing clear pathways for implementation. Their roadmap focuses on harnessing existing information to educate professionals and the public (2026), placing quality of life at the core of care prioritisation through standardised indicators (2030), and establishing Nordic clinical guidelines as a global model by 2040.
Inclusive Innovation Ecosystem
Mission Statement
By 2040, the Nordic health ecosystem will be globally recognised as a leader in equitable women's health innovation, fueled by open data, smart regulation, and aligned public-private investment. A unified framework will support technology enablers, risk-proportionate regulation, and public-private capital, enabling scalable solutions for women's health.
The Innovation group identified three key transformations. Technology as an enabler shifts from high-cost, siloed innovation to digital twins, citizen data, and advanced tools that make development faster, cheaper, and more inclusive. Smart regulation transforms compliance from a barrier into agile frameworks that balance safety with innovation support, making the Nordics globally competitive. Unified investment logic emerges from the first two transformations, moving from fragmented venture capital and government views that undervalue health to joint public-private investment, recognising health as a core societal and economic value. Their roadmap includes establishing clear funding rules (2026), centralising and unifying data collection and access to innovation (2030), and adopting a holistic perspective on health as a societal benefit by 2040.
Innovative Governance
Mission Statement
By 2040, Nordic governance reimagines health with trust, equality, and transparency at its core. New frameworks foster accountability across society, the economy, and healthcare, ensuring women enjoy healthy life years on par with men, with dignity, equity, and quality of life across all stages. Investing in women's health is an investment that reduces sick leave, increases workforce productivity, and strengthens national economies. The Nordics become the world's most trusted region for women's health, combining Nordic values, cutting-edge science, and innovation to create healthier lives for all.
The Governance group identified four transformations. Education and awareness as policy lever shifts from ad-hoc campaigns to mandated education pipelines with KPIs and accountability mechanisms. Institutionalised citizen participation and lived experience panels move from symbolic consultations with unclear influence to permanent panels embedded at every stage of decision-making. Data and measurability transformation requires moving from non-sex-disaggregated data to mandatory sex-disaggregated indicators for increased accountability. Resource allocation transformation demands shifting from episodic, siloed budgeting, fragmenting women's health, to life-cycle-based budgeting and investments incentivising prevention and innovation.
Health Literacy & Awareness
Mission Statement
By 2040, the Nordics will operate a life-course women's health literacy system that is normalised, evidence-based, and accessible in everyday life. Knowledge about women's health has become a shared cultural norm, empowering women and those around them to make informed decisions at every life stage, free from shame, stigma, and misinformation.
The Literacy & Awareness group identified cultural transformation as the foundation enabling all other missions. The education transformation shifts from a place of misinformation and outdated knowledge to trustworthy and transparent systems of knowledge generation proactively used by educators, doctors, and authority figures in collaboration with women and society. The cultural transformation moves from "prude to proud," replacing stigma with cultural awareness and openness. The access to information transformation evolves from disconnected, paywalled information with a culture of ignorance to communities that listen and trust, building transparent and accessible knowledge generation with a citizen-connected approach. By 2040, their vision is: "The Nordics are the new WHO" for women's health literacy standards.
Voices of Lived Experience
Throughout the workshop, participants shared their visions of 2040 through live polling, revealing what matters most: being heard and taken seriously when bringing health concerns to doctors; having personalised health data and technology to track hormonal trends; receiving preventative care before symptoms appear; experiencing no diagnostic delays or dismissals; talking freely about health issues without stigma; trusting bodily experience to be respected; not feeling guilty about being sick or in pain during periods. One participant captured the essence: "I have a manual to understand my body" and "I can trust my own experience to be respected." Another emphasised, "More money is spent on prevention than on treatment. This will fundamentally change the healthcare system (for everyone, not only women)." Above all, women envisioned feeling safe, valued, and able to simply live without constantly thinking about health challenges.
The Pattern of Convergence
Every group independently identified that current systems aren't just inadequate, they aren't designed for women. Research prioritises male-normed approaches, care measures survival over quality of life, innovation lacks clear investment signals, governance operates without adequate sex-disaggregated data, and culture maintains silence rather than openness. Yet beneath these critiques, something more significant emerged. When we mapped the specific activities each group proposed, the same infrastructure needs appeared repeatedly: education pipelines, funding mechanisms, policy frameworks, and data systems. Section 3.3 makes this convergence visible and shows how it led to the 3×4+1 framework that organises the rest of this Charter.
3.3Four Pillars for Aligned Action
The previous section presented each expert group's distinctive contribution. When we laid these outputs side by side and mapped specific activities, a striking pattern emerged: the same infrastructure needs appearing across all five groups, expressed through different lenses.
| People | Money | Policy | Data | |
|---|---|---|---|---|
| Research Group | Researchers trained in women's health methodology | Catalytic Fund €20M+€200M+ | Priority Framework mandates | Infrastructure & Standards (FAIR, cohorts) |
| Care Group | Education Ecosystem for HCPs and public | Value-based reimbursement linked to QoL | Clinical Guidelines (CVD, menopause, pain) | QoL measurement systems (PROMs) |
| Innovation Group | Data Ambassadors embedded in initiatives | 50% investment allocation requirement | Regulatory Sandbox for digital health | Intelligence Layer for AI interpretation |
| Governance Group | “Education as policy lever with KPIs” | “Lifecycle budgeting, resource allocation transformation” | “Permanent lived experience panels, governance frameworks” | “Mandatory sex-disaggregated data” |
| Literacy Group | Cultural transformation through education | Economic case showing ROI | Political legitimacy for mandates | Transparency driving data collection |
Table 2: Convergence Across Expert Groups
Read Horizontally
Each group's transformations require support from multiple pillars.
Read Vertically
Every pillar appears in multiple expert group outputs.
This overlap is evidence that we're looking at shared infrastructure, not competing priorities. The five groups weren't proposing five different systems, they were describing the same enabling infrastructure from five different angles.
3.4The Women’s Health 2040 Framework
The pattern of convergence revealed a cleaner structure: three operational domains sharing four infrastructure pillars, built on one enabling foundation. We call this the Women's Health 2040 Framework — a coordination map and menu of options that enables multiple pathways toward the 2040 Vision. The framework organises coordination opportunities without prescribing a single path. Institutions can engage with individual cells, entire pillars, or domain-specific strategies, choosing what fits their mandate and capacity.
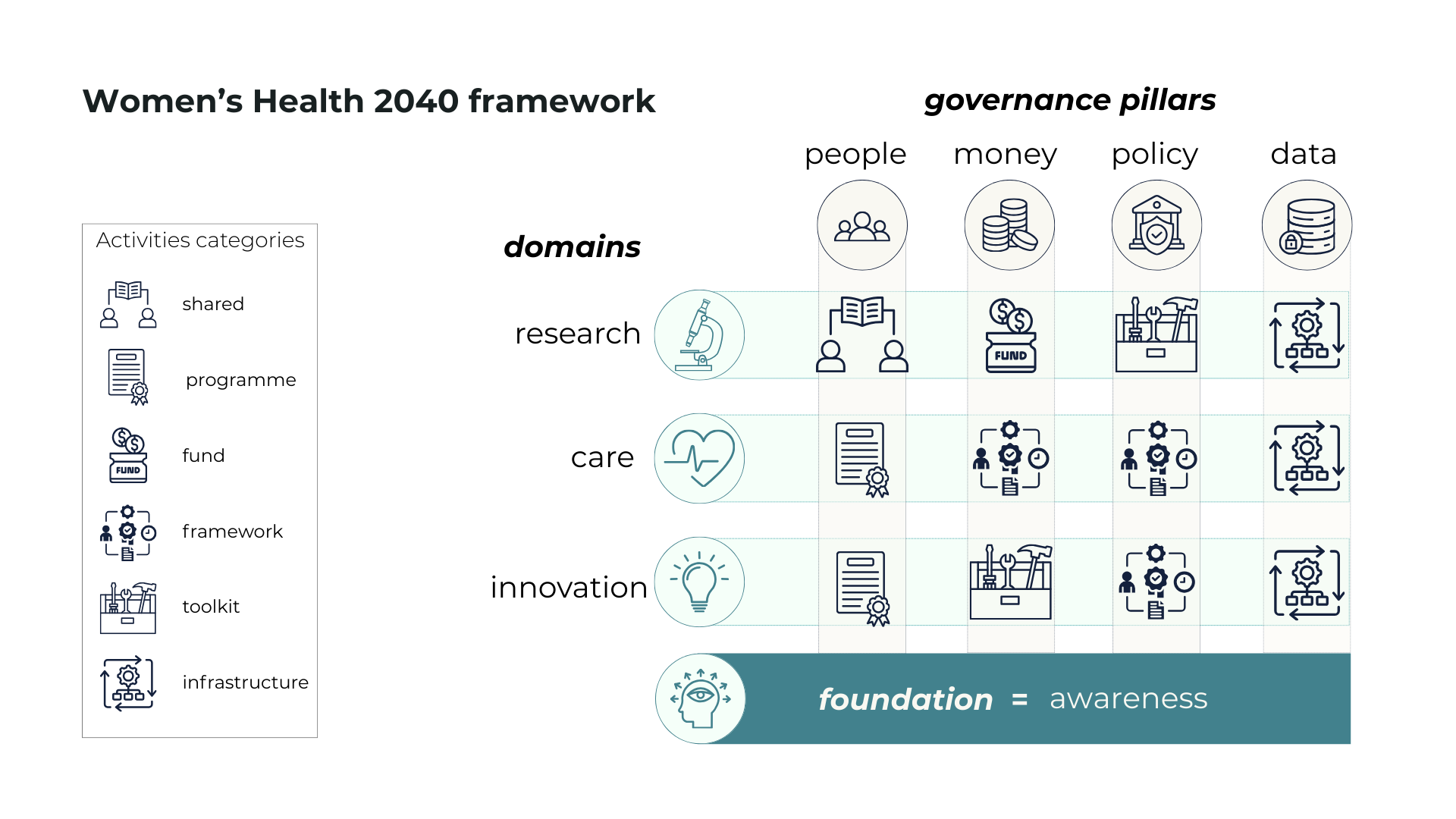
The Three Domains (Rows)
Research (Evidence Generation) creates the knowledge foundation, validating female physiology models, establishing sex-stratified clinical trial standards, and building longitudinal cohorts that track women's health across life stages.
Innovation (Scaling Solutions) translates evidence into accessible tools, developing digital health platforms, creating adaptive regulatory pathways, and building the data infrastructure that enables personalised, preventive care.
Care (Clinical Implementation) embeds improvements into daily practice by training healthcare professionals, establishing gender-sensitive clinical guidelines, and systematically measuring quality of life outcomes alongside survival metrics.
The Four Infrastructure Verticals (Columns)
People (Capacity & Training) builds human capability by training researchers in women's health methodology, educating healthcare professionals in gender-specific medicine, developing data ambassadors who integrate women's health requirements into innovation infrastructure, and transforming public understanding through coordinated literacy campaigns.
Money (Funding & Investment) aligns financial resources, coordinating research funding mechanisms, linking healthcare reimbursement to quality of life outcomes, establishing clear investment guidelines with allocation requirements, and implementing life-cycle budgeting that recognises women's health as long-term value creation rather than episodic cost.
Policy (Governance & Regulation) establishes enabling frameworks, mandating sex-disaggregation in research, developing gender-sensitive clinical guidelines, creating agile regulatory pathways for women's health innovations, and embedding permanent lived experience panels in decision-making structures.
Data (Infrastructure & Standards) creates shared systems, building standardised, interoperable registries with validated female health data, developing the Nordic Women's Health Intelligence Layer for innovation, collecting patient-reported outcomes systematically, and ensuring mandatory sex and gender-disaggregated reporting across all public data.
| People | Money | Policy | Data | |
|---|---|---|---|---|
| Research | Researchers trained in women's health methodology | Catalytic Fund + Priority Framework | Priority Framework (sex-stratified mandates) | Infrastructure & Standards (dictionary, cohorts, FAIR) |
| Care | Education Ecosystem (HCP + public training) | QoL Framework (value-based reimbursement) | Clinical Guidelines (gender-sensitive care) | QoL Framework (PROMs collection) |
| Innovation | Data Ambassadors (embed requirements in initiatives) | Investment Guidelines (50% allocation) | Regulatory Sandbox (adaptive regulation) | Intelligence Layer (AI infrastructure) |
Table 3: The Women’s Health 2040 Framework
The Foundation Layer
Awareness forms the foundation upon which all other infrastructure depends. Without cultural legitimacy and public understanding, political will to invest remains absent, demand for professional training never materialises, mandates lack public support, data transparency finds no champions, and accountability pressure fails to emerge. This foundation stems from coordinated public education campaigns, Parliamentary briefings demonstrating a return on investment, cultural normalisation efforts shifting from stigma to openness, and systematic work making the women's health gap visible and legitimate.
How The Women’s Health 2040 Framework Works
Each cell represents a specific mission that requires a particular infrastructure pillar. Some activities serve multiple functions; for example, the Care domain's Quality of Life Framework appears in Money (drives reimbursement), Data (collects patient-reported outcomes), and Policy (informs clinical guidelines). This isn't duplication; it shows activities that must be well-coordinated because they serve multiple purposes simultaneously.
Conversely, some cells remain intentionally sparse. Research doesn't build its own people infrastructure but relies on the shared education ecosystem that serves all missions. This efficiency is the matrix's strength: one coordinated data infrastructure with women's health requirements embedded serves all three missions rather than each building separate systems.
The framework functions as a coordination map and menu of options. It enables multiple pathways: coordinated Nordic strategy development, bilateral or regional collaboration, institutional initiative selection, or funding alignment. No single coordination body is required, though the framework supports coordinated action when institutions choose to pursue it. The detailed mapping of initiatives within each matrix intersection, along with implementation guidance, continues as the next phase of Charter development.
The framework's power lies in its ability to show how infrastructure serves multiple missions simultaneously. Two examples illustrate this principle in practice: how governance functions across all three domains, and how literacy serves as the enabling foundation beneath them all.
3.5Spotlight: Why Governance Became a Pillar, Not a Domain
The Governance group identified four infrastructure transformations that Research, Care, and Innovation all require. Rather than constituting a separate mission, these became the Governance and Regulation pillar that enables coordinated action.
Life-cycle budgeting replaces episodic, siloed funding. In Research, this shifts investment from treating late-stage disease to preventing onset, funding longitudinal cohorts that track women across decades rather than single intervention studies. In Care, reimbursement structures reward prevention and improvements in quality of life rather than reactive crisis management. In Innovation, investors recognise women's health as a long-term value creation rather than a focus on quarterly returns, enabling development timelines that align with biological reality rather than venture capital expectations.
Mandatory sex-disaggregated data creates accountability. In Research, this mandate ensures clinical trials report outcomes by sex, making invisible biases visible. In Care, it reveals diagnostic delays and treatment disparities that aggregate data obscures. In Innovation, disaggregated effectiveness data shows which solutions genuinely work for women versus which optimise for male-normed metrics.
Institutionalised lived experience panels are embedded at every decision stage. In Research, women with endometriosis, PCOS, and cardiovascular disease shape priority-setting rather than researchers alone determining agendas. In Care, panels ensure clinical guidelines reflect actual patient journeys, identifying where pathways dismiss symptoms or delay diagnosis. In Innovation, panels become mandatory regulatory checkpoints, testing whether technologies improve lives or digitise existing bias.
Education pipelines with KPIs build capacity systematically. Cross-ministry collaboration ensures Research funders, Care providers, and Innovation regulators all understand female physiology and can identify gender bias in their domains.
This is why Governance isn't a fourth mission, it's the Governance and Regulation infrastructure that makes coordinated action possible. The group's vision, "ensure women live as many healthy years as men", requires governance frameworks that serve all three missions simultaneously.
If governance demonstrates how infrastructure enables coordinated action across missions, literacy reveals something even more fundamental: the cultural conditions that determine whether any infrastructure succeeds at all.
Key Metric
To make the Policy pillar operational, the Nordics can anchor governance in existing global standards and measurement frameworks. But for these tools to accelerate rather than restrict progress in women's health, governance needs to reflect the realities of those driving change. That means aligning standards with the operational constraints of startups, the due-diligence needs of investors, and the validation practices of patient groups. If these perspectives are ignored, frameworks become unusable in real-world sandboxes, commercialisation pathways, or community adoption.
The Women's Health Impact Tracking Platform (WHIT) offers a structured way to see where women are underserved across conditions, life stages, and socio-economic groups, and quantifies the economic cost of inaction. Integrating WHIT into Nordic governance would support life-cycle budgeting and create a common baseline for tracking the region's core outcome: how many healthy lived years women gain by 2040.
The SAGER Guidelines provide a globally recognised benchmark for sex- and gender-specific reporting in research. Making SAGER the minimum Nordic requirement removes ambiguity for funders, ethics bodies, journals, and researchers, ensuring that sex-disaggregated data is mandatory, consistent, and globally interoperable.
The Hologic Global Women's Health Index offers an external benchmark for how women actually experience health and wellbeing. Linking Nordic KPIs to this index would reveal strengths, expose gaps internal metrics miss, and ground progress in lived-experience data that directly influences healthy lived years.
Together, WHIT, SAGER, and the Hologic Index translate governance from principle into practice. They create shared metrics, reduce fragmentation, and strengthen the governance infrastructure that Research, Care, and Innovation all rely on, with healthy lived years as the ultimate measure of success.
3.6Spotlight: Awareness as Foundation
The Literacy & Awareness group captured their vision: "Cycle-synched organisations are twice as effective; the Nordics are the new WHO." This wasn't a separate domain but the foundation determining whether the technical infrastructure succeeds or remains aspirational.
Their insight: transformation requires moving from "prude to proud", replacing stigma with cultural awareness where understanding women's health becomes a shared social norm, not a women-only topic. This cultural shift must happen with women as co-creators, not just recipients.
Consider why the Infrastructure & Standards requires this foundation. Building the Nordic Women's Health Intelligence Layer depends on women contributing intimate health data across decades. But trust emerges only through transparent governance, public education showing how data improves care, and cultural normalisation. Without Awareness, data infrastructure remains technically perfect but practically empty because women won't share data in systems they don't trust.
The same dynamic appears in Funding and Investment pillar. Life-cycle budgeting requires political commitment to survive electoral cycles. Politicians allocate resources where constituents demand action. That demand emerges from Parliamentary briefings demonstrating ROI, public campaigns making the health gap visible, and economic narratives showing health as a societal asset. The group emphasised corporate accountability, large employers publishing women's health literacy KPIs to normalise workplace support. Without this foundation, funding commitments dissolve when budgets tighten.
In PEOPLE, their emphasis on mandated education pipelines across schools, universities, workplaces, and clinical re-credentialing creates the human capacity all domains need. Training educators, doctors, and authority figures in trustworthy knowledge systems, with plain-language, free, multilingual resources through community channels, builds a health-literate society where gender-aware decisions become the norm.
Their roadmap included immediate wins (Nordic literacy standards, curriculum integration) and transformational goals (becoming global standard-setters). The Literacy group showed that knowledge and awareness aren't parallel efforts; it's the cultural legitimacy that determines whether People's capacity gets built, Money flows consistently, Policy gain public support, and Data systems earn trust.
These examples demonstrate why the framework is organised as it is: three operational domains requiring four shared infrastructure pillars, all resting on a foundation of knowledge and cultural legitimacy. The structure isn't theoretical; it emerged directly from what +50 experts identified as necessary for transformation. Part 4 explores how organisations can engage with this framework, choosing pathways that match their context, capacity, and strategic priorities.
Key Metric
A key enabler is a Nordic Health Literacy Index, co-developed with the Nordic Council of Ministers for Health and Social Affairs, NOMESCO/NOSOSCO, and the Nordic Welfare Centre. Unlike traditional literacy measures, this Index would capture citizens' ability to access, understand, and act on health information through digital, cultural, and gender lenses. It would expose where inequities persist—across age groups, workplaces, life stages, and communities—and anchor literacy as a shared governance priority rather than a communications effort. By embedding the Index within existing Nordic statistical structures, it becomes a formal accountability mechanism: ministries, municipalities, employers, and healthcare providers can track progress, direct resources, and benchmark themselves publicly. Without such a metric, cultural change stays aspirational; with it, health literacy becomes measurable, fundable, and foundational to every other domain.

Part 4
Pathways Forward
4.1Multiple Ways to Use This Framework
The Women's Health 2040 Framework functions as a guiding document, not a prescription. Institutions can engage through multiple pathways, each valid on its own terms and adaptable to the operational realities of startups, the due-diligence needs of investors, and the validation practices of patient organisations.
Coordinated Nordic Strategy Development
The framework enables joint action when institutions choose alignment. Research councils could coordinate funding mechanisms, pooling resources to achieve proportional allocation. Health ministries could harmonise clinical guidelines, ensuring gender-sensitive care becomes the Nordic standard. Innovation agencies could align regulatory sandboxes, reducing fragmentation for startups that otherwise face five different pathways to approval. Including investors and patient groups here ensures that standards are commercially realistic, investable, and grounded in lived-experience validation rather than purely top-down governance.
Bilateral or Regional Collaboration
Two or three countries can pursue targeted coordination without requiring unanimous agreement. Partners might jointly develop data infrastructure, establishing standards and interoperability that others adopt when ready. Others could pilot value-based reimbursement models that link payment to healthy lived years. Startups benefit from these regional pilots because they reduce regulatory uncertainty, while investors gain clearer signals of where future markets are emerging. Patient organisations provide feedback loops that ensure pilots address real needs, not hypothetical ones.
Institutional Initiative Selection
Individual institutions can identify entry points within the matrix independently. A research council might establish sex-stratification mandates. A hospital could implement quality-of-life measurement. An innovation agency could launch a Data Ambassador training programme. Startups might test new technologies within aligned sandboxes. Investors could use the matrix to evaluate which innovations have systemic relevance. Patient organisations can use it to identify where their input shapes development and implementation. Coordination emerges from aligned action within a shared framework, not from centralised planning.
Funding Alignment
Funders can use the matrix to identify investment priorities and areas of opportunity. The framework illustrates where coordinated funding unlocks systemic change and where targeted investments facilitate specific progress, ensuring resources flow toward enabling infrastructure rather than being fragmented across disconnected projects.
The Strength Lies in Flexibility
When institutions work within a shared framework, their independent actions compound because they're building the same infrastructure system. Coordination emerges from the framework itself.
4.2Next Steps
This Charter establishes the coordination framework, comprising The Women's Health 2040 Framework structure, engagement pathways, and foundation layer. The framework is immediately usable by institutions seeking to align their strategies, identify opportunities for collaboration, or justify investments.
The Work Continues
The detailed mapping remains to be done, involving the identification of initiatives within each matrix intersection, determining which existing Nordic and European efforts already address specific needs, identifying where gaps require new investment, and understanding how coordination mechanisms function in practice. The next edition of The Nordic Charter for Women's Health 2040 will provide the actionable roadmap that institutions require for implementation.
Until that mapping is available, institutions can begin immediate engagement. Research councils can establish mandates and coordinate funding discussions to ensure effective allocation of resources. Health systems can pilot measurement frameworks. Innovation agencies can launch training programmes and regulatory sandboxes. Education ministries can mandate curriculum integration. Each initiative strengthens the infrastructure system that all domains require.
Living Framework
The Charter functions as a public good; no single institution owns it. As institutions engage, their experiences will refine what works, reveal challenges, and identify new opportunities for coordination. The framework evolves through use, ensuring it remains relevant to institutional realities.
The Nordic Opportunity
Women's health represents a defining choice for the Nordic region. The status quo lowers healthy life expectancy for women, diagnostic delays spanning years, and research excluding female physiology is neither inevitable nor acceptable. The region possesses everything needed: world-class institutions, universal healthcare, strong governance traditions, and populations demanding evidence-based equality.
What has been missing is a coordination infrastructure. This Charter provides that framework. The pathway from fragmented efforts to systematic transformation is now visible. What remains is the collective will to pursue what 136 stakeholders envisioned: a future where women's health becomes a birthright, not a benefit, and where the Nordics demonstrate what equitable, integrated, life-course health systems can achieve.
4.3Commitment to the Nordic Charter for Women’s Health 2040
The Nordic Charter for Women's Health 2040 sets a shared direction for a future where women's health is understood as foundational to societal resilience, economic strength, and everyday wellbeing. It offers a common framework that institutions may use to align their efforts, coordinate investments, and build the systems required for change.
By signing this Charter, institutions signal their support for the vision, principles, and transformation pathways outlined in the document. Signing is voluntary and non-binding. It reflects a commitment to contribute, within each institution's mandate and capacity, to advancing women's health across the Nordic region.
This shared commitment strengthens collective action. It acknowledges that progress depends on broad collaboration across sectors: from research and education to care systems, innovation ecosystems, policymaking, investment, and civil society. Signing the Charter is a step toward sustained, long-term alignment that enables the Nordics to lead globally on equitable, evidence-based women's health.





